What is Food intolerance ?
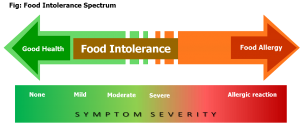
Food intolerance is relatively a new concept, and can be difficult to understand. Even most doctors have a poor understanding of it, particularly when there is a mixture of signs and symptoms that do not belong in the same disease group or there is no pathological explanation. Common complaints such as headaches, bloating and tiredness …


