What are FODMAPs?
FODMAPs are short chain carbohydrates and sugar alcohols naturally occurring in foods or as an additive. As a group they are known as FODMAPs (Fermentable Oliogosaccharides, Disaccharides, Monosaccharides and Polyols). Not all carbohydrates are considered FODMAPs and the content level also varies.
Collectively they have three common properties:
- Incomplete digestion and absorption. They can be classified into two groups;
- Those that are partly absorbed FODMAPs (fructose, lactose polyols)
- Those which are not absorbed in anyone (fructans and galactooligosaccharides)
- Osmotically active action drawing in water into the large bowel.
- Rapidly fermented by bacteria due to their short chain molecular structure.
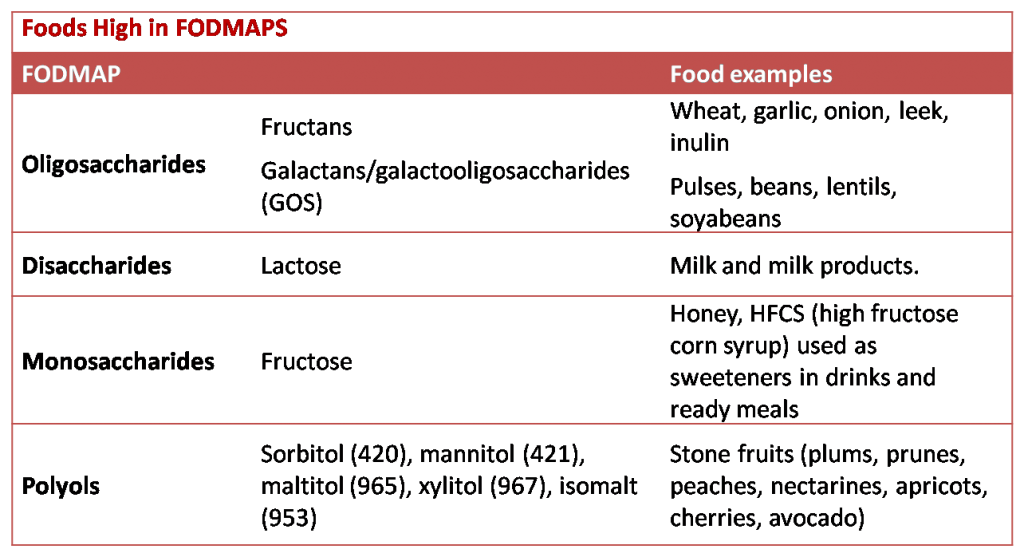
Low FODMAP diets are scientifically proven and was first pioneered in Melboune, Australia for the management of IBS. However, in the UK it is still a relatively new concept. The effectiveness of FODMAP diets is variable. In people with IBS it is around 70%. All FODMAPs have a role in symptom development, but the dietary amount varies across the different genetic, ethnic and dietary groups. For example people who can digest lactose, dairy products are not a problem. Fructans and fructose are most common in North American, Western and European diets. Furthermore, we have to consider that the rate of absorption of fructose in the small intestine is widely variable and consequently the effects experienced by different people will also vary.
How do FODMAPs affect the bowel?
Luminal distension is considered to be the common physiological cause of many functional gut disorders. It induces symptoms of pain, bloating and abdominal distension. This evidence comes from Barostat and gas infusion research studies. FODMAP food that has not been digested passes through the small intestine to the colon where they are fermented by the bacteria resulting in the release of gas causing bloating, wind and pain. Due to their osmotic nature water enters the colon resulting in loose motions and diarrhoea. Research has shown that in individuals with sensitive bowel function (e.g. IBS) FODMAPs tend to react more readily.
What can I do to find out what if FODMAPs affect me?
If you have gastrointestinal symptoms, diarrhoea, constipation, gas, bloating and/or cramping then you are more likely to be sensitive to the effects of FODMAPs. Reduce your intake of high FODMAP foods for 4-8 weeks and observe whether your symptoms improve. If they do then you can start to reintroduce some of the higher FODMAP food one at a time to see if your symptoms recur. You can track your symptoms in a diary or use a symptom tracker app. The lists below will also be helpful.
Resources:
- The Monash University Low FODMAP Diet Department of Gastroenterology, Monash University. http://www.med.monash.edu/cecs/gastro/fodmap/low-high.html
- GESA, DHF (2013). Low FODMAP diet. http://www.gesa.org.au/files/editor_upload/File/Consumer%20Brochures/2014/Low%20FODMAP%20Diet.pdf
- Kate Scarlata (2014). Low FODMAP diet checklist. http://blog.katescarlata.com/wp-content/uploads/2011/04/LOWFODMAPCHECKLIST_lowfodmap_oct15-1.pdf
- Low FODMAP diet (Stanford hospital & clinics) https://stanfordhealthcare.org/content/dam/SHC/for-patients-component/programs-services/clinical-nutrition-services/docs/pdf-lowfodmapdiet.pdf
- Barrett J.S. (2013).“Extending Our Knowledge of Fermentable, Short Chain Carbohydrates for Managing Gastrointestinal Symptoms” Nutrition in Clinical Practice. 28(3) 300-306.
- Gibson P R, Shepard S J. (2010) Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach. J of gastroenterology and hepatology. 25(2) 252-258.
